How Stress Affects Your Hormones and Menstrual Cycle
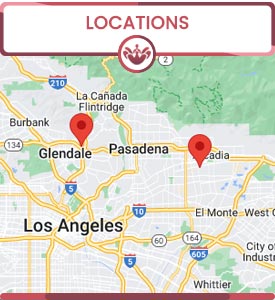
At The OB-Gyn & Incontinence Center, Dr. Prema Kothandaraman explains how stress can significantly impact your hormones and menstrual cycle. Stress can lead to hormonal imbalances, causing irregular periods, heavier bleeding, or even missed cycles. Dr. Kothandaraman offers personalized care to help manage stress-related hormonal changes and guide you toward achieving a balanced, healthy cycle through lifestyle adjustments, stress management techniques, and appropriate medical interventions. For more information, contact us or book an appointment online. We have convenient locations to serve you.


Table of Contents:
How does stress impact my hormones?
Can stress delay my period?
Can stress cause mood swings during my period?
What is the relationship between stress and PMS (premenstrual syndrome)?
We understand that stress is more than just an emotional experience—it can have real, physical effects on your body, especially your hormonal and reproductive health. When you’re under stress, your body activates the hypothalamic-pituitary-adrenal (HPA) axis, leading to increased levels of stress hormones like cortisol and adrenaline.
For women, persistently high cortisol can disrupt the delicate balance of reproductive hormones such as estrogen and progesterone. This disruption may lead to menstrual irregularities, fertility challenges, and even exacerbate symptoms of menopause or polycystic ovary syndrome (PCOS). Many women also experience decreased libido and mood changes, as stress can affect neurotransmitters like serotonin and dopamine.
Importantly, stress can also impact pelvic health. Elevated cortisol levels may worsen symptoms of urinary incontinence by increasing muscle tension or altering bladder function. Women who are already managing conditions such as overactive bladder or stress urinary incontinence may notice their symptoms intensify during periods of heightened stress.
Additionally, chronic stress can weaken your immune system, making you more susceptible to infections, including urinary tract and vaginal infections.
Managing stress is not only crucial for your overall well-being—it’s an essential part of maintaining hormonal balance and supporting your gynecological and pelvic health. We encourage our patients to adopt healthy lifestyle habits, engage in relaxation techniques, and seek support when needed. Our team is here to help you address both the physical and emotional aspects of your health, so you can feel your best—inside and out.
We often see patients concerned about changes in their menstrual cycle. One common culprit is stress. When you experience significant physical or emotional stress, your body releases hormones like cortisol. These stress hormones can disrupt the normal function of the hypothalamus—a part of the brain that regulates your menstrual cycle by communicating with the pituitary gland and the ovaries. This disruption can lead to delayed ovulation or even skipped periods.
Both short-term stress (such as a major life event or sudden changes in routine) and chronic stress can impact your menstrual cycle. Prolonged stress may cause your periods to become irregular over several months. Other factors, including illness, weight fluctuations, excessive exercise, or underlying gynecological conditions, can also influence your period.
If you notice that your period is consistently late or irregular and you’re feeling stressed, it’s important to address both your stress and your menstrual health. Managing stress through exercise, mindfulness, or support from a healthcare provider can help restore normal cycles. However, ongoing irregularities may point to other health concerns such as polycystic ovary syndrome (PCOS), thyroid disorders, or other gynecological conditions.
When you’re under stress, your body releases hormones like cortisol and adrenaline. These stress hormones can interact with the natural fluctuations of estrogen and progesterone that occur throughout your menstrual cycle. This interaction can heighten emotional responses, making you feel more irritable, anxious, or sad than usual—especially during your period.
Many women already experience mood changes as a normal part of their cycle. Adding stress into the mix can make these symptoms more pronounced and even affect your daily life. We encourage our patients to practice stress management techniques such as relaxation exercises, regular physical activity, and healthy sleep habits. These strategies can help balance your mood and improve your overall well-being.
If you find that mood swings during your period are severe or interfering with your quality of life, please don’t hesitate to reach out to us. Our experienced providers can help evaluate your symptoms, discuss treatment options, and offer support tailored to your needs. Your emotional health is just as important as your physical health, and we’re here to help you achieve balance every step of the way.
We understand that premenstrual syndrome (PMS) is more than just a monthly inconvenience—it can significantly impact your physical, emotional, and behavioral health. PMS describes a group of symptoms that occur in the days leading up to your period, including mood swings, irritability, anxiety, fatigue, and physical discomfort.
The Stress–PMS Connection
Research has shown a strong link between stress and PMS. Increased stress levels can make PMS symptoms worse and even increase your chances of experiencing them. This is due to stress hormones like cortisol and adrenaline, which interact with the natural hormonal changes—such as fluctuations in estrogen and progesterone—that occur throughout your menstrual cycle. This interaction can intensify PMS symptoms and may also affect sleep, appetite, pain sensitivity, and emotional well-being. We recognize that chronic stress can also alter the way your brain processes hormonal changes, making some individuals more sensitive to PMS symptoms month after month.
Comprehensive Care for PMS and Your Well-Being
Our team takes a holistic approach to women’s health, including the management of PMS and related symptoms. We encourage patients to discuss their stress levels and emotional health with us, as addressing stress is an essential part of managing PMS and improving overall quality of life. Effective stress management techniques—such as regular exercise, relaxation exercises, and mindfulness—can help reduce the severity of PMS symptoms.
If you are struggling with PMS, stress, or related concerns like urinary incontinence, our experienced providers are here to help. Together, we can create a personalized plan to support your physical and emotional well-being throughout your menstrual cycle. For more information, contact us today or book an appointment online. We have convenient locations to serve you in Arcadia, CA, and Glendale, CA. We serve patients from Arcadia CA, Glendale CA, Monrovia CA, Pasadena CA, Los Angeles CA, Burbank CA, and surrounding areas.


Additional Services You May Need
▸ Urogynecology
▸ Minimally Invasive Gynecology
▸ Monalisa & Medical Aesthetics
▸ Bioidentical Hormone Replacement Therapy
▸ Urinary Incontinence
▸ Pelvic Organ Prolapse
▸ Painful Bladder
▸ Urinary Tract Infection
▸ Genitourinary Syndrome of Menopause
▸ Female Sexual Dysfunction
▸ Urinary Retention
▸ Vaginal Laxity & Prolapse
▸ Postpartum Pelvic Floor Problems
▸ PCOD
▸ Bladder Prolapse Repair
▸ Urgent PC
▸ Fibroids
▸ Excessive Bleeding
▸ Pelvic Pain
▸ Birth Control & IUD
▸ Vaginal & Pelvic Infection
▸ Monalisa Touch
▸ STD
▸ TempsureVitalia
▸ Biote Pellet Therapy
▸ Topical BHRT
▸ Flexsure
▸ Rectal Prolapse Repair
▸ Tempsure ENVI
▸ Minimally Invasive Pelvic Surgery for Incontinence